In this topic
PBS claim weekly payment cycle
Medicare claim statements to help you reconcile
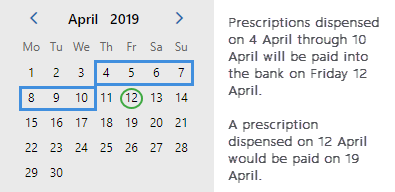
PBS claim weekly payment cycle
- The payment period runs from Thursday to Wednesday.
- Payment for each period is made on a Friday. Payments are made every Friday, for every pharmacy.
From 21 March 2019, the minimum lag time on payments has been reduced from nine days to two days. This means that the new lag time can range between two days and nine days.
Your claim will be easier to reconcile if you close it on a Wednesday night, so that the claim cycle and payment cycle finish on the same day.
Example
Medicare claim statements to help you reconcile
Medicare will provide you with a weekly, mailed payment advice, and an electronic statement.
Payment advice
Every week, Medicare will mail you a payment advice document, which summarises what they have paid you.
Notes
- Bank Reference Number: This is the RBA number that matches to your bank statement.
- The PBS Payment ID column usually shows one ID for each day of dispensing.
- In the CPN Subtotals Summary, the total Friday payment is broken down by claim period.

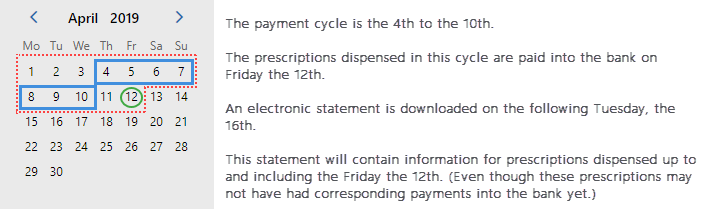
Electronic Statement
Every Tuesday, Medicare will send you an electronic statement. This automatically downloaded to Fred Dispense.
Electronic statements contain information not only for the period that has been paid, but up to and including the Friday of the last payment.
Electronic statements contain information not only for the period that has been paid, but up to and including the Friday of the last payment.
Example
Request a statement manually
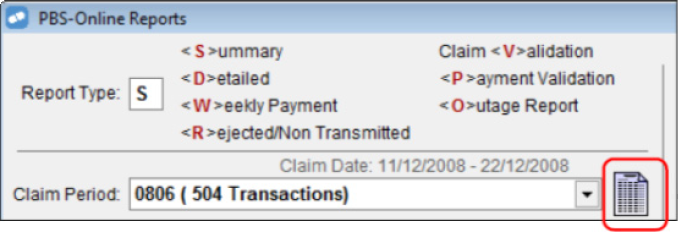
On the PBS Online Report Parameters screen, click the Statement icon.
Statement status
A statement status can be either Interim or Complete.
- Interim statements contain information for only part of the claim. Each interim statement for a claim period supersedes the last interim statement
- Complete statements are issued once paper prescriptions have been received by Medicare Australia and the final payment for that claim period has been made. The complete statement supersedes all interim statements.

Reports to help you reconcile your PBS statement
To access these reports: In Fred Dispense, from the Activities menu, select Pharmpay Claim, then select PBS Online Report Parameters.
Shows a summary of the statement data that has been downloaded.
For details, seeClaim Summary Report
Use to reconcile at an individual script level. Shows statement data that has been downloaded and allows you to filter by claim period, RBA number and payment ID.
For details, see Claim Detailed Report.
Use to identify which scripts have been paid in a weekly payment. Shows statement data that has been downloaded, Fred Dispense claim data, and downloaded statement data. You can filter the report by RBA number and payment ID.
For details, see Weekly Payment Report.
Shows prescriptions that have either been rejected or have not been transmitted to Medicare, based on Fred Dispense claim data and downloaded statement data.
You must generate this report before closing the claim so that any problem prescriptions can be corrected or re-transmitted.
For details, see Rejected / Non-Transmitted Scripts Report.
Identifies problem prescriptions in the current claim period. Use this report to correct any problems prior to generating and finalising the claim.
For details, see Claim Validation Report.
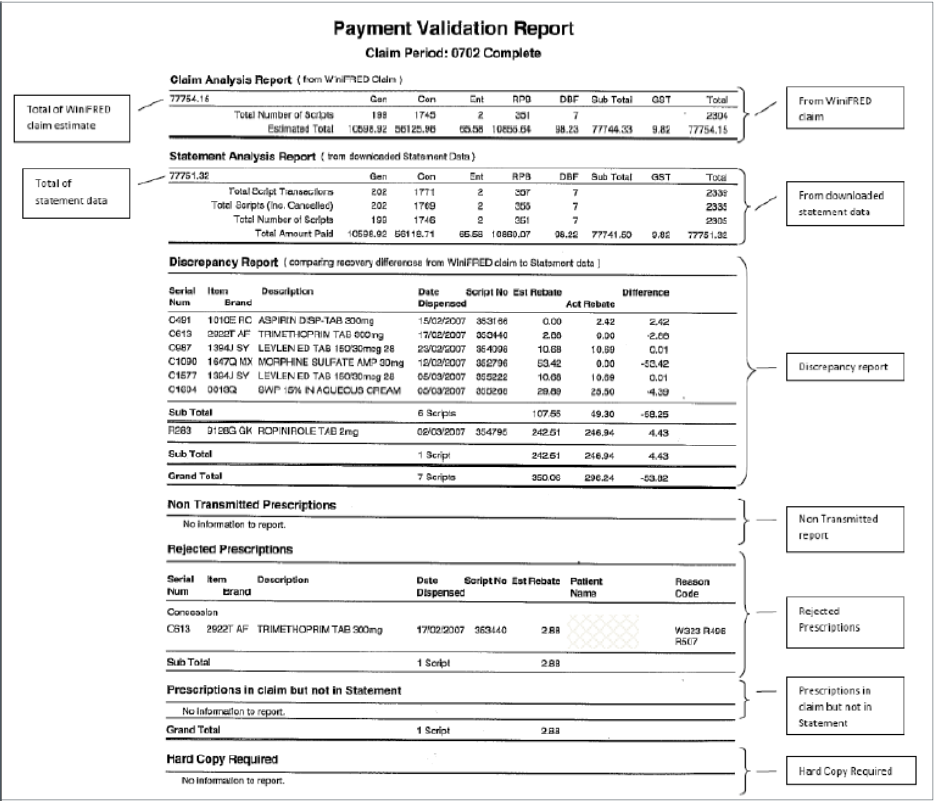
Displays claim analysis data from Fred Dispense; statement data from Medicare Australia, and any other irregularities.
This is the recommended report to use when reconciling your claim.
The Payment Validation report compares Fred Dispense data with downloaded statement data. The report is composed of the following sub-reports:
|
Choose this report… |
To… |
|---|---|
|
Claim Analysis report |
Show the Fred Dispense claim estimated payments. |
|
Statement Analysis report |
Show all the statement information that has been downloaded. |
|
Discrepancy report |
Show the differences between the Fred Dispense data and the statement data downloaded from Medicare. |
|
Non-transmitted prescriptions |
Show any prescriptions that have not been transmitted to Medicare. |
|
Rejected prescriptions |
Show any prescriptions that have been rejected by Medicare. |
|
Prescriptions in claim but not in statement |
Show prescriptions that appear in the Fred Dispense Claim Analysis report but have no corresponding electronic statement data downloaded. This section may contain many prescriptions if the report is generated before any statement data is due to be downloaded. |
|
Hard Copy Required |
Show the prescriptions Medicare need a hard copy of before approving payment. |
Click the thumbnail below to see a larger image.
For details, see Payment Validation Report.
Shows prescriptions with specific processing codes that were received during a PBS Online outage.
Bundle prescriptions in this report separately when organising prescriptions to be sent in the claim.
These prescriptions have the processing code 02 and may have the following rejection codes:
|
Rejection Code |
Meaning |
|---|---|
|
R115 |
The entitlement number provided does not exist |
|
R116 |
The entitlement number provided is not current at date of supply |
|
R117 |
The entitlement number provided is no longer current at date of supply |
|
R359 |
Centrelink has advised that entitlement number provided is not current at date of supply |
For details, see PBS Online Outage Report.
Reconciling
The recommended method to reconcile PBS Online is to use the Payment Validation report to:
- Show what Fred Dispense estimates the payment for a claim period should be.
- Show what information has been downloaded in the electronic statement (paid or due to be paid).
- View any prescriptions in the claim that are not on the statement, to see what prescriptions are missing from the downloaded Medicare data when compared to your Fred Dispense data.
- Consider the payment cycle when interpreting this report. For what period has the information been downloaded? Is the statement Interim or Complete?
Verify whether prescriptions have been approved for payment
- If the statement data has been downloaded from Medicare for a specific prescription, it is shown in theDetailed Report.
- If the prescription has been paid it will have an RBA (bank reference) number.
Identify why you haven’t been paid for a prescription
- Run the Rejected/Non-transmitted Report and the Claim Validation Report for the required claim period to see if the prescription is rejected or not transmitted.
- If the prescription returned a message from Medicare stating [HardCopyRequired] then Medicare will not approve payment for this item until they view the paper prescription.
- If you are still unsure as to why you have not received payment, contact the Medicare processing department.
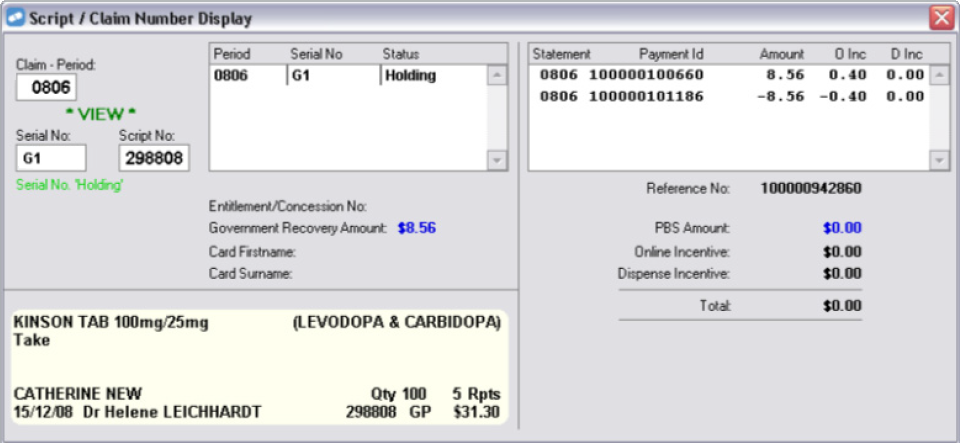
Get information about individual prescriptions
You can also obtain further information about individual prescriptions by viewing the script in Script Claim number display.
From the Activities menu, select Pharmpay Claim, then select Script Claim Number Display.
In the example (below) the prescription G1 in Claim Period 806 was claimed and then placed on hold. Therefore, the payment was reversed by Medicare.