Payment Validation Report
The Payment Validation Report assists you in reconciling your Medicare Australia claim payments against what has been dispensed in the claim.
The report compares the Fred Dispense Claim Analysis estimate with the payment information downloaded in statements from Medicare Australia.
Non-transmitted prescriptions, rejected prescriptions, prescriptions found to be in the claim but not in a statement and prescriptions that have received an online response of ‘Hard Copy Required’ are also reported.
PB50 information is optional and can be included by ticking the ‘Include PB50 Section’ prior to generating the Payment Validation Report.
-
From the Activities menu, select Pharmpay Claim, then PBS-Online Report Parameters.
Shortcut: Press [Alt+C], then [B].
The PBS-Online Reports popup displays.

- In the Report Type field, enter P.
- Select the Claim Period that you want to report on.
- (Optional) Select Include PB50 Section to include PB50 information for the selected claim.
-
To run the report, select OK.
Click the thumbnail below to see a larger image.
Breakdown of the Payment Validation Report
See below for an explanation of the different sections of the Payment Validation Report.
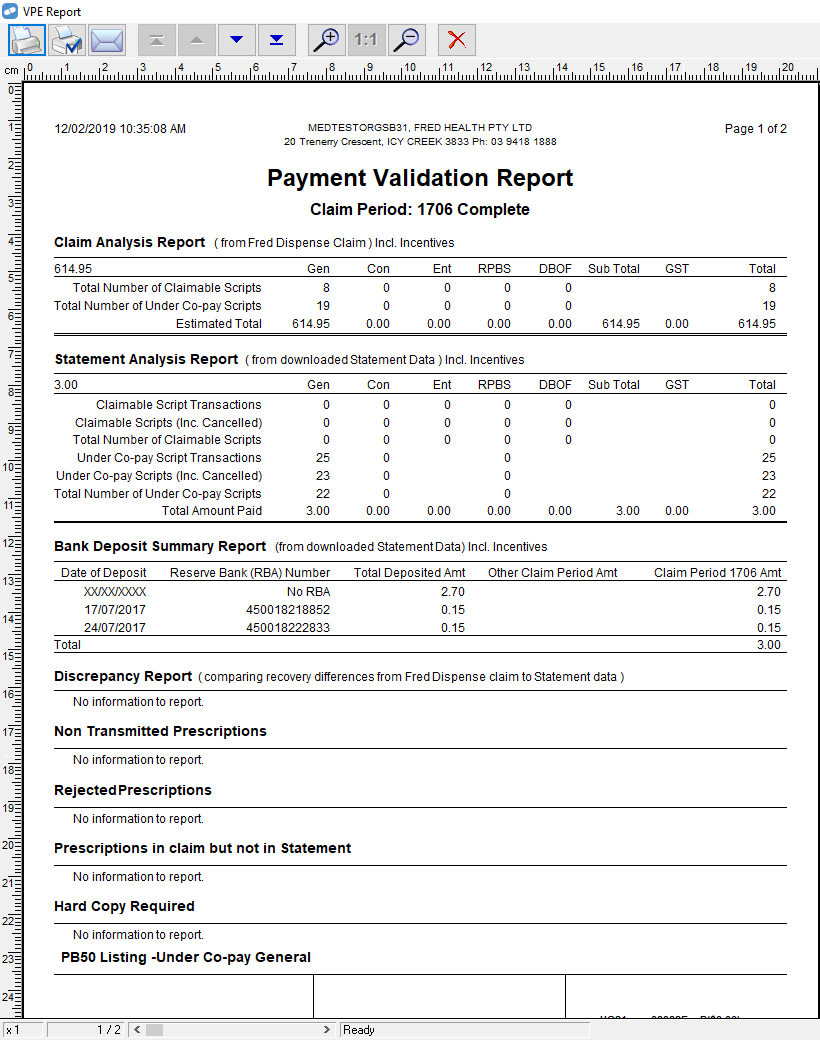
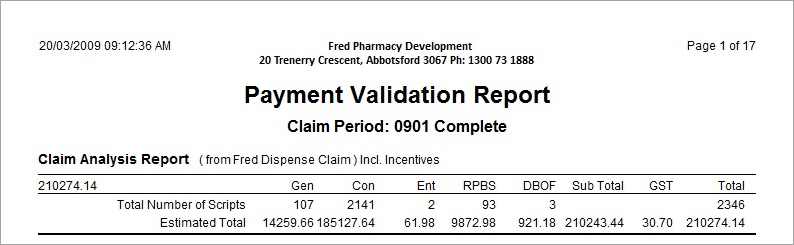
Claim Analysis Report
This section contains information from the Fred Dispense Claim Analysis Report. This is a summary of the claimable items that have been dispensed in the Fred Dispense program.
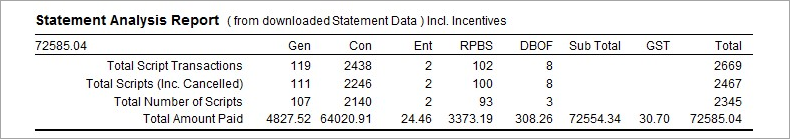
Statement Analysis Report
This section shows a summary of the information downloaded in the statement from Medicare Australia.
Each time a prescription is transmitted (i.e. dispensed, edited, reclaimed, cancelled) this counts as a transaction. The total script transactions is NOT indicative of how many individual scripts have been dispensed. For this figure you need to look at Total Number of Scripts.
Bank Deposit Summary Report
This section shows the amounts paid during the selected claim period. The payments are listed including the RBA number. This bank reference number can be used to reconcile the payments against what appears on your bank statement.
Payments can be made for claimable items from more than one claim. The ‘Other Claim Period Amt’ column shows how much of the payment is for scripts from another claim.
In this example we are shown an amount of $535.90 is for claimable items not in claim period 0901.

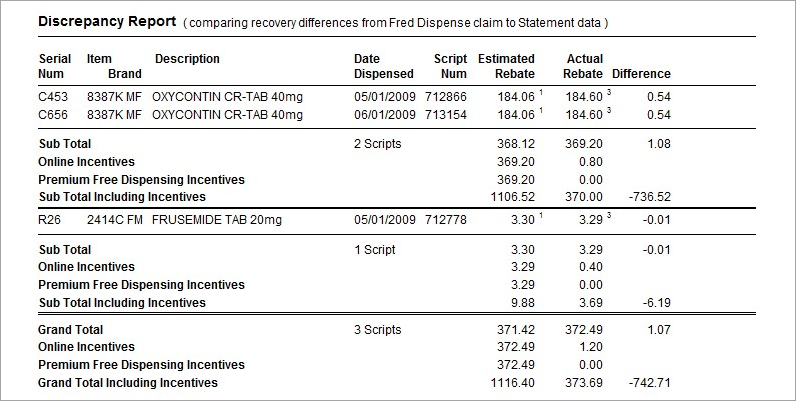
Discrepancy Report
The Discrepancy Report compares the payments estimated by Fred Dispense with the actual amounts paid in the statement downloaded from Medicare Australia. Any differences between these two reports are shown in the Discrepancy Report.
In the example below, the Fred Dispense estimated rebate for Oxycontin Cr-Tab 40mg is $184.06. The Actual Rebate from Medicare Australia is $184.60 resulting in a difference of 54 cents.
The discrepancies are sub totalled by claim category. A grand total of the discrepancies are also included.
Non Transmitted Prescriptions
Any claimable items that have not been transmitted will be shown here.

Rejected Prescriptions
Any claimable items that have been rejected will be shown here.

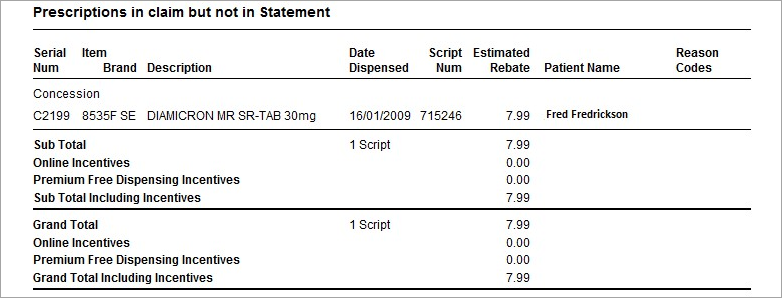
Prescriptions in claim but not in Statement
It is important to note that until the statement is complete this information cannot be considered final. There may be prescriptions listed as not in statement simply because the statement has not yet been downloaded from Medicare Australia for these items.
Hard Copy Required
This section lists any prescriptions for which the hard copy of the script is required prior to payment.

PB50 Listing
In this section each claimable script is listed with the serial number, NHS code and government recovery amount. Each claim category is shown separately.
Where there’s a gap in serial numbers, the claimable prescription for this serial number has been removed from the claim. For example the script may have been cancelled or reclaimed into a later claim period. (In the example below this would be G32 and G47)
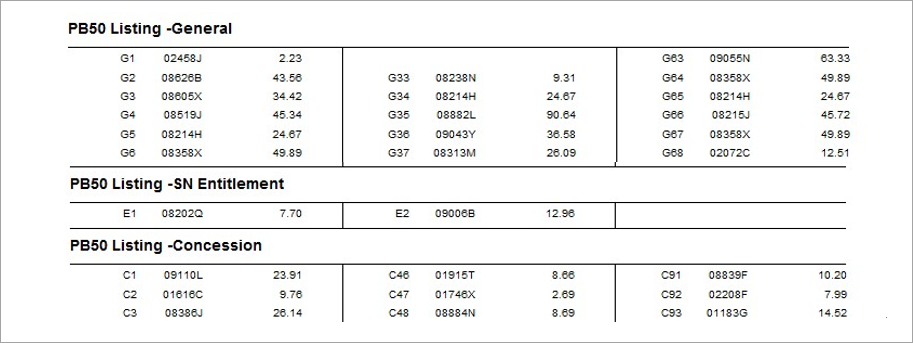
Parts of the report have been removed to reduce size.
Where an item is rejected, the text displays as bold. The price is shown in brackets and is preceded by an ‘R’. This is used to show that the claimable item received a rejection. The value of this rejected item is displayed in the brackets
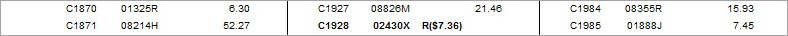
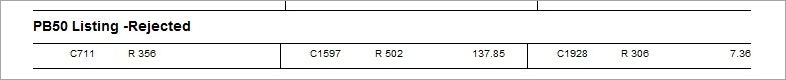
PB50 Listing Rejected
At the end of the report a summary of all rejected scripts is displayed.