Dispense a Continued Dispensing Supply
In order to provide a Continued Dispensing supply, the pharmacist must be satisfied that the patient has previously had the medicine prescribed; therapy is stable and the prescribe has performed clinical review that supports continuation of the medicine; and the medicine is safe and appropriate for the patient.
Prerequisite: Add your AHPRA Number to the Pharmacist Details
Before you can completed and successfully claim a Continued Dispensing Supply, your AHPRA number must be recorded in Fred Dispense.
If your AHPRA number is not recorded in Fred Dispense, you may receive a PBS warning 'W 044 The prescriber number provided is invalid' for the prescription.
- Select (Lists menu > Pharmacists).
- Add the 10-digit AHPRA Number.
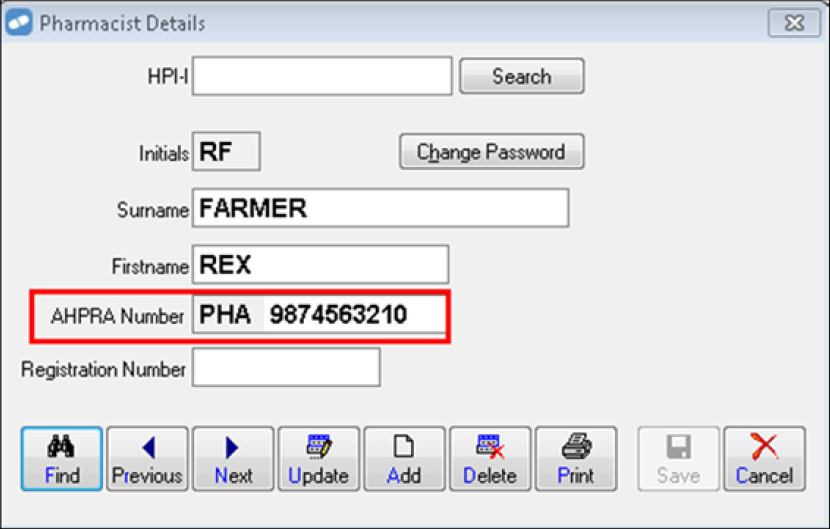
- Select Save.
All leading zeros must be entered in the AHPRA Number field. Fred Dispense ony validates that the supplied AHPRA Number has the correct number of digits.
How to Dispense a Continued Dispensing Supply
Medicare will cross-check other pharmacies for Continued Dispensing claims and will reject payment for a claim if the supply has already occurred in the last 12 months.
-
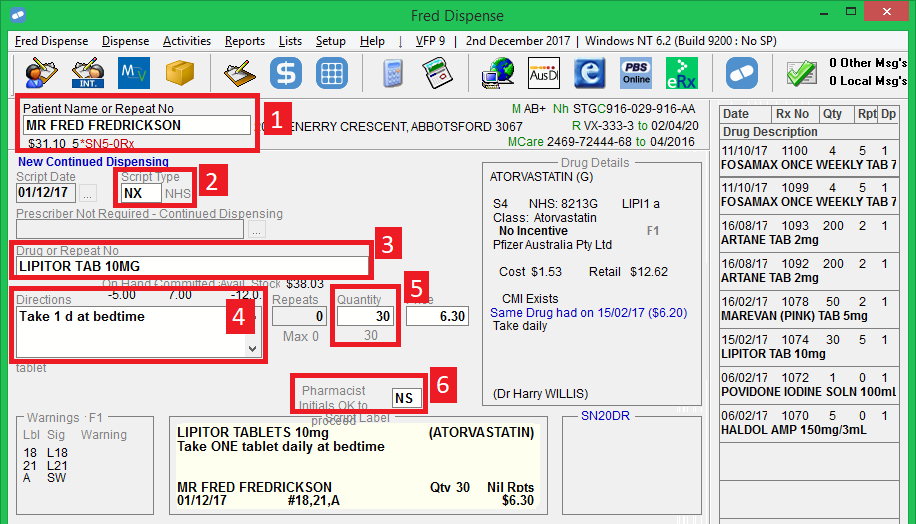
Select the Patient.
-
In the Script Type field, enter NX (NHS) or RX (Repat).
The Script Date defaults to today’s date and becomes read-only. The Prescriber No. field is disabled.
-
Select the Drug.
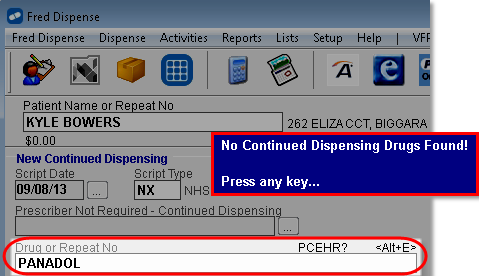
PBS medicines eligible for Continued Dispensing are currently limited to oral hormonal contraceptives, and statins. If you select a drug inelibible for Continued Dispensing, a blue message is displayed.
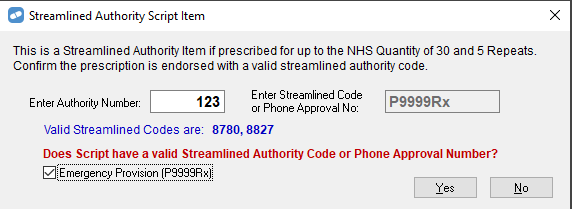
When dispensing eligible authority items, please remember to use 123 as the authority number and select the Emergency Provision (P9999Rx) check box.
The Repeats field is disabled and set to 0.
Repeats are disabled because only one Continued Dispensing supply is allowed per patient, per eligible medicine, per year. A valid prescription is required for any subsequent dispensing of this drug to this patient in the next 12 months.
-
Enter the Directions.
-
Enter the Quantity.
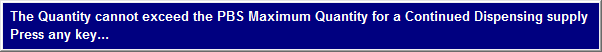
The quantity defaults to the PBS maximum quantity. It can be reduced but not exceeded. If you enter a higher quantity than the PBS maximum, a blue message is displayed.
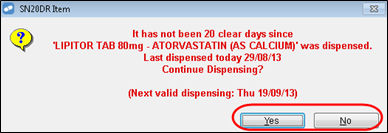
Deferring does not apply to Continued Dispensing. Where Regulation 25 and Safety Net Consequences apply for the supply, Fred Dispense displays a modified SN20DR Item dialog prompt, excluding the Defer option.
Where only Regulation 25 rules apply to the Continued Dispensing supply, Fred Dispense displays a modified Clear Days dialog prompt, excluding the Defer option.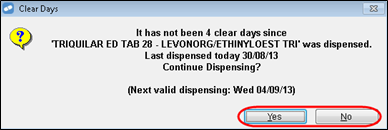
Click Yes to continue, or No to cancel dispensing.
PBS claiming rules remain unchanged. -
Enter your Pharmacist Initials.
Fred Dispense prints a modified repeat form (for claiming purposes), three Consumer Declaration and Prescriber Notification forms, and the label(s) for the medication.
- Ensure the repeat form and the Consumer Declaration and Prescriber Notification forms are signed and dated and handled as required. For details, see Continued Dispensing Forms.
Other information relating to Continued Dispensing
- Owing does not apply to Continued Dispensing, but a Continued Dispensing supply can be edited and set to Owing, if it is rejected by Medicare.
- The maximum PBS quantity cannot be exceeded and the pharmacist cannot use an Authority number to override the maximum PBS quantity.