July 2024
News
In this issue
| What's New in Fred Dispense |
|
| Fee changes applicable from 1 July 2024 |
|
| End of financial year and stocktaking help |
|
| Catch up with the Fred team this August! |
|
| This Month's PBS Changes |
|
What's New in Fred Dispense
Expanded access to the CTG PBS Co-Payment Program Under the CTG PBS Co-Payment Program from 2024-25 Budget.
Prior to July 2024, Eligible First Nations patients who:
-
Normally paid the full PBS co-payment of $31.60 got their medicine at the concession price of $7.70.
-
Normally paid the concession price got PBS medicines for free.
Additionally, the CTG PBS Co-Payment currently only applied to section 85 PBS medicines supplied by community pharmacies, approved medical practitioners or private hospitals.
This included eligible section 85 medicines supplied under Continued Dispensing arrangements.
From July 1, 2024, this measure expands access to the CTG PBS Co-Payment Program to:
-
Apply to section 100 PBS medicines when dispensed by a community pharmacy, approved medical practitioner or private hospital.
These changes will also include both section 85 and section 100 PBS medicines supplied under Continued Dispensing arrangements.
This allows eligible First Nations patients access to the full suite of PBS section 85 and section 100 medicines in both primary and acute care settings.
It will ensure First Nations patients will pay the same reduced cost for their PBS medicines to support continuity of care regardless of treatment setting.
60 Day Dispensing – Reporting
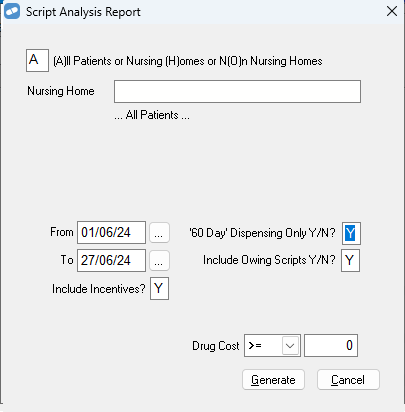
The Script Analysis Report now has been modified to enable you to report on 60 day dispense items only. This is achieved by selecting Y to ’60 Day’ Dispensing Only Y/N? prior to generating your script analysis report as seen below.
This report will assist with estimating** your Additional Community Supply Support Payment (ACSSP) (announced as part of 8CPA).
The ACSSP is comprised of two components which will be provided by Services Australia in the form of manual payments:
-
Component 1 $4.79 per dispense (2 months supply - 60 day dispensing that are claimable) S85 Drugs only.
-
Component 2 $0.78 per dispense (ALL claimable dispensings) S85 Drugs only.
These component payments do NOT apply to under copay prescriptions nor drugs within Section 100 of the PBS Schedule.
-
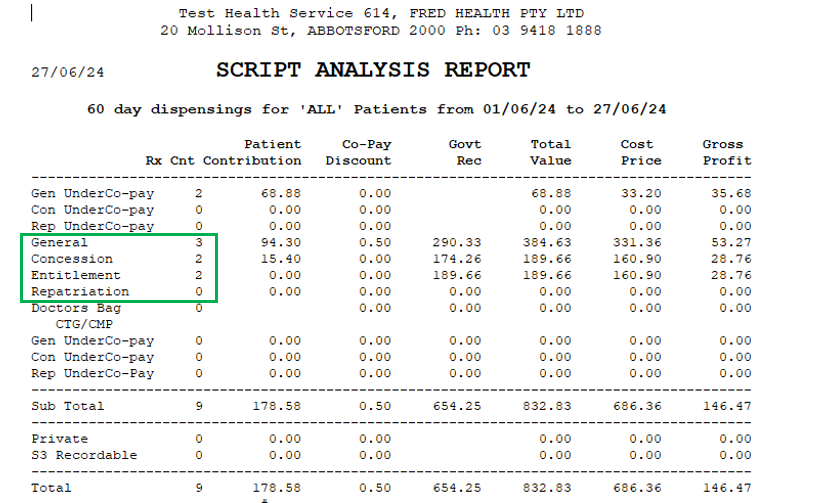
Component 1 can be calculated by running the script analysis report, filtered for 60 Day dispensing for the applicable date range then multiplying the count of all the claimable scripts by $4.79.
In the example below the estimated Component 1 payment would be 7x $4.79 ($33.53).
-
Component 2 rough** estimate would be calculated by re running the Script Analysis report without filtering (selecting N to ’60 Day’ Dispensing Only Y/N?).
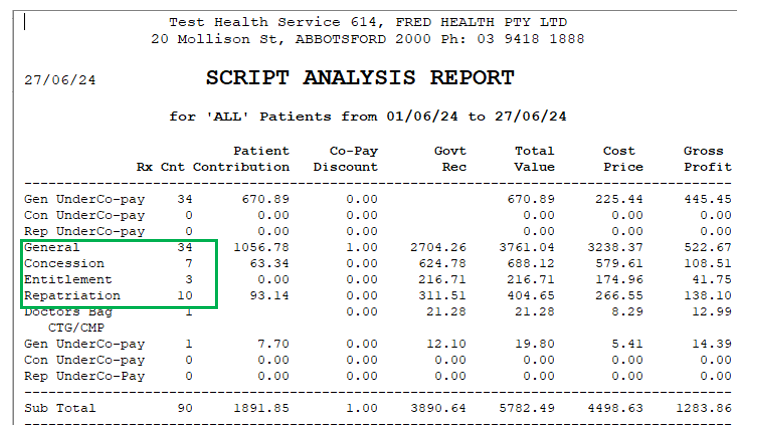
The estimation would be calculated as total count of claimable scripts, in this case 54 (34 +7+3+10) multiplied by $0.78 = $42.12**
Therefore total expected payment in my example would be $33.53+$42.12= $75.65.
** The component 2 calculation would be inflated as the count would include Section 100 drugs if applicable. This is a temporary solution to assist in the short term, further refinements will be provided in a future update to take into account dispensing of claimable Section 100 medicines.
Fee changes applicable from 1 July 2024
Fees
The following fees, patient contributions, and Safety Net thresholds apply from 1 July 2024 and are included, where applicable, in prices published in the Schedule.
|
Fee Type |
Fee |
|
|---|---|---|
|
Dispensing Fees |
Ready-prepared |
$8.67 |
|
Dangerous drug fee |
$5.37 |
|
|
Extemporaneously-prepared |
$10.71 |
|
|
Allowable additional patient charge* |
$3.45 |
|
|
Additional Fees (for safety net prices) |
Ready-prepared |
$1.45 |
|
Extemporaneously-prepared |
$1.87 |
|
|
Patient Co-payments |
General |
$31.60 |
|
Concessional |
$7.70 |
|
|
Safety Net Thresholds |
General |
$1647.90 |
|
Concessional |
$277.20 |
|
|
Safety Net Card Issue Fee |
$12.04 |
|
* The allowable additional patient charge is a discretionary charge to general patients if a pharmaceutical item has a dispensed price for maximum quantity less than the general patient co-payment. The pharmacist may charge general patients the allowable additional fee but the fee cannot take the cost of the prescription above the general patient co-payment for the medicine. This fee does not count towards the Safety Net threshold.
End of financial year and stocktaking help
It's nearly time for End of Financial Year Reporting and Stocktaking. To assist you with these processes, refer to the following Fred Office Plus resources:
Important reminder for department stocktakes
If you plan to do a department stocktake, make sure that all product items are assigned to a department. Otherwise, items will be missing from your stock count.
- Select Reporting > Inventory Reports > Item Pricing Details.
- Click Open Report.
- Select the No Department checkbox and then click Run Report.
- For each product item in the list, assign it to a department:
- Double click an item to display the stock card.
- Select a Department.
- Click Save and Close.
As a shortcut, you can do this in bulk using the Quick Action Wizard. Select multiple lines, then right-click, select Perform Quick Action and then follow the steps in the Wizard.

UPGRADE TO THE NEW FRED MOBILITY
Now on an advanced Android platform with a familiar and modern interface, navigation and workflow.
Contact your local Fred representative or sales@fred.com.au
This Month's PBS Changes
For the full Schedule of Pharmaceutical Benefits, go to the PBS website at http://www.pbs.gov.au/ where you can search the schedule by drug name.
For your convenience, we've also uploaded a printable summary of this month's important PBS changes to this site.
For Highly Specialised Drugs (HSD) items (CAR and non-CAR), please refer to the Schedule of Pharmaceutical Benefits as well as Services Australia to confirm whether the PBS item code for a HSD is eligible to be dispensed and claimed by your pharmacy type.

